
Cholesterol 101: Everything You Need to Know (And Then Some!)
CONFUSED ABOUT CHOLESTEROL? YOU’RE NOT ALONE!
High cholesterol and the health issues it causes are major concerns in today’s society, yet we’re constantly bombarded with conflicting advice.
Supplements, fad diets, detox plans, high-fat versus low-fat, dirty keto—you name it! No wonder it’s hard to know which direction to take…
But with heart disease being one of the leading causes of death worldwide, it’s crucial to get the right information. Fortunately, when we dive into the science and consult experts, the picture starts to become clearer, with consistent recommendations emerging across the globe. The good news? Lifestyle changes can be incredibly effective at lowering cholesterol and improving overall health.
Let’s take a closer look and break it all down. 😊
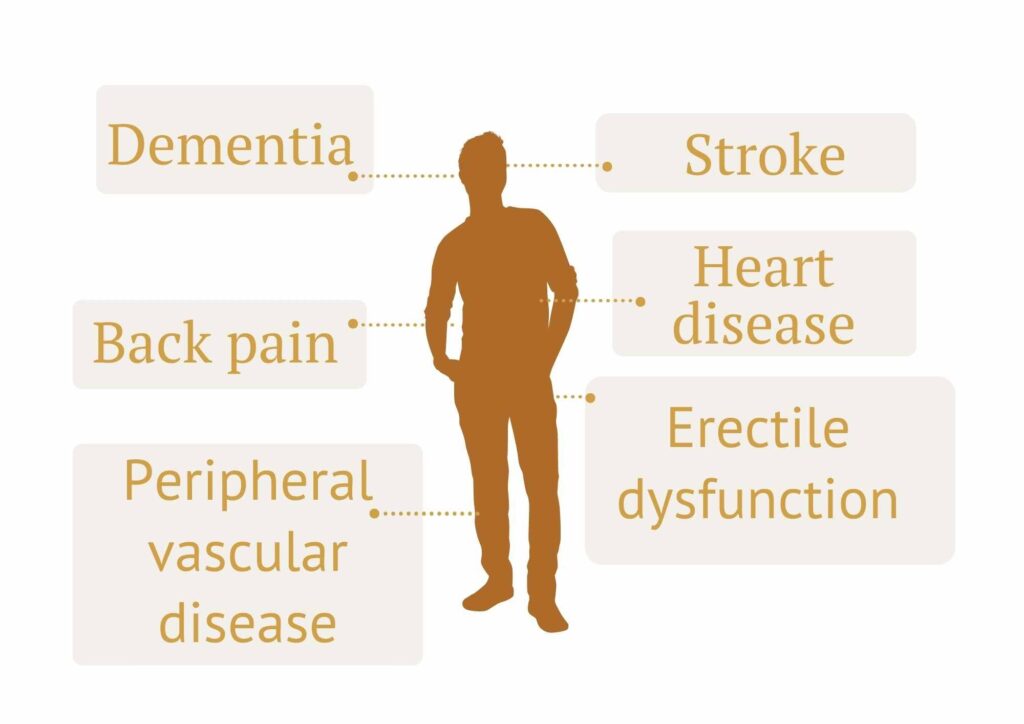
Random Fact: Did you know that raised cholesterol doesn’t just increase the risk of heart disease? It’s also linked to strokes, erectile dysfunction, Alzheimer’s, and even back pain and injuries! 😳
And while many people believe genetics are the main culprit, studies show that they only account for about 10-20% of the total heart attack risk. This means that lifestyle factors, like diet and exercise, play the biggest role in influencing both cholesterol levels and heart health.
Cholesterol isn’t just a concern as we get older either. Autopsies of soldiers in their 20s and 30s have revealed early cholesterol plaques, and some plaques have even been found in kids as young as 11! That’s why countries like the USA recommend checking cholesterol levels starting at age 9. 😬
But here’s the interesting part: in regions where people eat whole food, plant-focused diets and stay active, heart disease and cholesterol-related problems are virtually nonexistent.
This demonstrates just how powerful diet and lifestyle can be in preventing these issues. This is something we dive deeper into in our Nutrition Focus and Reboot courses.
So, the takeaway? It’s never too early to start being proactive about your health!
WHAT IS CHOLESTEROL, ANYWAY?
Cholesterol is a yellow, waxy substance that’s technically a type of fat, alongside saturated fat, unsaturated fat, and triglycerides.
It’s measured through blood tests, and it plays a key role in assessing vascular health— with research consistently showing cholesterol levels are directly linked to the risk of heart attacks, strokes, and other cardiovascular issues.
In other words, the worse your cholesterol readings are, the higher your risk for these problems (although other factors like high blood pressure, diabetes, and metabolic syndrome also play an important role).
We do need some cholesterol to build cell walls, protect nerve sheaths, and produce key hormones like estrogen, testosterone, vitamin D, and bile acids (needed for digesting fats).
However, too much cholesterol can be harmful. Our liver can usually make all the cholesterol we need, so we don’t actually need to consume it through our diet!
This is where balance comes in—just like most things in life, we need enough cholesterol, but not too much. We’ll dive deeper into why that’s important in the next section.
Another crucial aspect of cholesterol is not just how much we have, but where we store it in the body. When cholesterol is inside the liver, it’s being used for those essential functions mentioned above. But when it ends up clogging our arteries, that’s when we run into trouble.
Fun fact: cholesterol is only found in animal products. This is why those on plant-based diets tend to have much lower cholesterol levels overall, along with lower rates of cholesterol-related health problems.
It’s also why whole food, plant-focused diets (like the ones we promote in our courses) are recommended by health experts around the world for better heart and brain health.
We’ll talk more about how different foods affect cholesterol levels in just a moment, but first, let’s take a look at what makes cholesterol “good” or “bad.”

ALL ABOUT GOOD AND BAD CHOLESTEROL – LETS BREAK IT DOWN
If you’ve had a cholesterol test, you’ve probably heard terms like “good” and “bad” cholesterol. These refer to HDL and LDL cholesterol. While there are more subtypes within these groups, we’ll stick to the basics for now.
What Are HDL and LDL?
Interestingly, HDL and LDL aren’t actually cholesterol themselves—they’re lipoproteins, which act as carriers to transport cholesterol through your bloodstream. Since blood is mostly water and fat doesn’t mix with water, lipoproteins are essential for moving cholesterol where it needs to go.
HDL (High-Density Lipoprotein)
Often called the “good” cholesterol, HDL carries cholesterol away from artery walls and tissues back to the liver, where it can be reused or removed from the body. Think of HDL as the clean-up crew, ensuring cholesterol is sent to the right place.
Because of its role in protecting against heart disease, higher levels of HDL are considered beneficial. We’ll cover strategies to boost HDL later in this post.
LDL (Low-Density Lipoprotein)
On the other hand, LDL is known as the “bad” cholesterol. It transports cholesterol to places you don’t want it, such as the walls of your arteries, where it can accumulate and form plaques. These blockages can restrict blood flow to critical areas like your heart, brain, and other organs, increasing the risk of heart attacks, strokes, and more.
Research consistently shows that high LDL levels are strongly linked to heart disease and other related conditions.
In fact, decades of studies confirm that lowering LDL can significantly reduce the risk of these issues – for every 1% reduction in LDL cholesterol, your risk of heart disease decreases by 2%!
High LDL levels are also associated with other conditions like osteoarthritis, autoimmune diseases, and certain women’s health issues. Although the reasons aren’t fully understood, it’s likely that lifestyle changes targeting LDL also influence these other conditions.
Triglycerides (TGL): The Other Cholesterol Type
Triglycerides are another type of fat measured in standard cholesterol tests, but they’re different from HDL and LDL.
Triglycerides are in essence, an energy storage mechanism for our body. When you consume more calories than your body needs, your liver converts the excess into triglycerides, which are stored in fat cells as an energy reserve. Later, when your body requires extra energy, these triglycerides are released into your bloodstream to fuel your muscles, generate heat, and keep your cells running.
This system works well when there’s balance, and has been essential for human survival when food sources were scare. But when we consistently consume more calories than we burn, triglyceride levels can become too high, spilling over into the bloodstream.
High triglyceride levels often signal that the body is struggling to manage energy intake. They are strongly associated with insulin resistance (a precursor to type 2 diabetes) – to learn more about this check out our article on insulin resistance.
Elevated triglyceride levels mainly come from excess calories, especially those from added sugars, refined carbohydrates, alcohol, and overeating.
By understanding the roles of HDL, LDL, and triglycerides—and how they interact—you can take meaningful steps toward improving your heart health. For a deeper dive into cholesterol and practical strategies for better health, check out our Nutrition and Reboot courses.

WHAT SHOULD MY CHOLESTEROL READING LOOK LIKE?
For the general population in New Zealand, the recommended cholesterol levels are:
- Total cholesterol: Less than 4 mmol/L
- LDL cholesterol (bad cholesterol): Less than 2 mmol/L
- Triglycerides: Less than 1.7 mmol/L
- HDL cholesterol (good cholesterol): Greater than 1 mmol/L
- Total cholesterol:HDL ratio: Less than 4
- Triglyceride to HDL ratio: Ideal is less than 0.87; above 1.74 is too high (A lower TG:HDL ratio is better and indicates improved insulin sensitivity and lower cardiovascular risk)
It’s important to note that often the PATTERN of cholesterol levels is almost as important as the separate numbers in isolation! Ie its not just your total cholesterol level that matters, it’s how this is broken down into different types of cholesterol – for the reasons we’ve just covered.
An important pattern to be aware of though, is a combination of high triglycerides, high LDL, low HDL, and elevated insulin levels
This can be a marker of a condition known as metabolic syndrome, which dramatically increases the risk of heart attacks and strokes. If you see this pattern on your blood tests, talk to your doctor about a full heart health checkup!
These targets can vary based on your overall health though, for example, if you have a history of heart disease, strokes, or other conditions that increase your cardiovascular risk, your LDL target may be much lower—sometimes as low as 1.4 mmol/L.
To determine the healthiest cholesterol levels for you, it’s essential to get a personalised cardiovascular risk assessment with your doctor. They can help tailor recommendations to your unique health profile.
WHY DOES CHOLESTEROL EVEN MATTER?
This is the million dollar question – after all, why talk about cholesterol at all, unless we talk about why it’s important to our health!
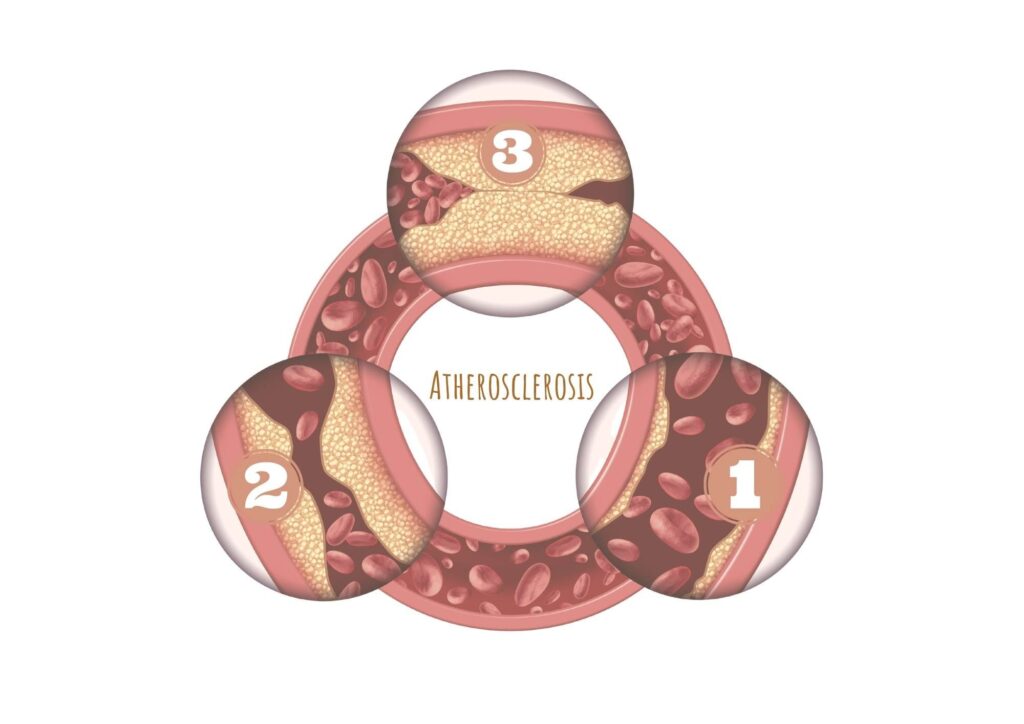
The key lies in a process called atherosclerosis—a slow, progressive condition that can begin as early as childhood or young adulthood and often goes unnoticed for decades.
When levels of LDL cholesterol, and other small dense cholesterol particles (often referred to as “bad” cholesterols) become too high, these molecules transport cholesterol to the walls of your blood vessels (arteries). There, the cholesterol gets deposited in the inner lining (endothelium) of the arteries, forming blockages known as plaques.
This build-up of plaque is what defines atherosclerosis. Over time, the plaques can grow, progressively narrowing the arteries and reducing blood flow.
Imagine a cross-section of an artery:
- Stage 1: Early plaque build-up begins, with cholesterol starting to accumulate.
- Stage 2: Plaques grow, narrowing the artery and slowing blood flow.
- Stage 3: Advanced disease occurs, where plaques significantly obstruct blood flow or even rupture, causing heart attacks or strokes.
This gradual process highlights why managing cholesterol levels early in life is essential—it helps prevent serious complications long before they appear.
HOW DO CHOLESTEROL PLAQUES CAUSE PROBLEMS?
Once cholesterol plaques form, they can lead to health issues in two main ways:
1) Plaque Rupture and Blood Clots (Thrombosis)
Initially, cholesterol plaques are covered by a protective “cap,” which hardens over time and becomes calcified. This stable plaque causes gradual artery narrowing and can be measured using tests like CT calcium scoring.
Stable plaques are less likely to cause immediate harm since they don’t typically lead to heart attacks or strokes. However, when the plaque becomes inflamed and the cap cracks, it triggers the release of chemicals that promote blood clot formation (thrombosis).
If a clot forms on the surface of the ruptured plaque, it can partially or fully block the artery, cutting off blood flow to the tissue it supplies. This blockage can lead to:
- Heart attack: If it happens in heart arteries.
- Stroke: If it occurs in brain arteries.
- Other tissue damage: Blockages can also affect the limbs (limb ischemia), intestines (mesenteric ischemia), or eyes (retinal artery occlusion).
The likelihood of plaque rupture depends on many factors, including inflammation, which makes the blood vessels “stickier” and more prone to clotting.
Risk factors for plaque rupture include:
- Chronic inflammation (measured by tests like hs-CRP).
- Conditions like diabetes, hypertension, autoimmune diseases (e.g., rheumatoid arthritis, lupus), and sleep apnea.
- Lifestyle factors like smoking, obesity, and diets high in saturated fats, processed foods, and animal protein.
Following an anti-inflammatory eating pattern and addressing these risk factors can reduce your risk of plaque rupture and clot formation.
2) Gradual Artery Narrowing (Stable Plaques)
If the plaque remains stable and doesn’t rupture, it can still gradually narrow the artery over time. This reduces blood flow to tissues, causing symptoms that worsen as the narrowing progresses.
Unlike ruptured plaques, stable plaques don’t fully block blood flow, so symptoms often appear during activity (when tissues need more blood) and improve with rest.
Symptoms depend on where the narrowing occurs:
- Heart: Leads to stable angina (chest pain during exercise due to reduced blood supply to the heart muscle).
- Legs: Causes peripheral vascular disease, leading to leg pain while walking.
- Brain: Can result in vascular dementia, a common type of dementia caused by reduced blood flow to the brain.
- Genitalia: Can cause erectile dysfunction, often an early sign of arterial narrowing years before other symptoms develop.
- Spine: Reduced blood flow to spinal discs may cause back pain or disc degeneration (disc prolapse).
The Bottom Line:
Both plaque rupture and gradual narrowing can have serious consequences, but they’re also preventable. Managing cholesterol, reducing inflammation, and adopting a heart-healthy lifestyle can go a long way in protecting your arteries and overall health.
Want to dive deeper into preventing and managing these risks? Check out our Nutrition and Reboot courses.
PREVENTING AND MANAGING ATHEROSCLEROSIS (BLOCKED ARTERIES) – THE POWER OF LIFESTYLE
Preventing atherosclerosis before it starts is the ideal approach. However, even when blockages have begun, adopting a healthier lifestyle can still make a significant difference. It’s never too late to take action!
Lifestyle changes can:
- Improve symptoms.
- Reduce the risk of heart attacks and strokes.
- Even extend life expectancy.
In some cases, studies have shown that atherosclerosis can reverse with intensive lifestyle interventions. 😊

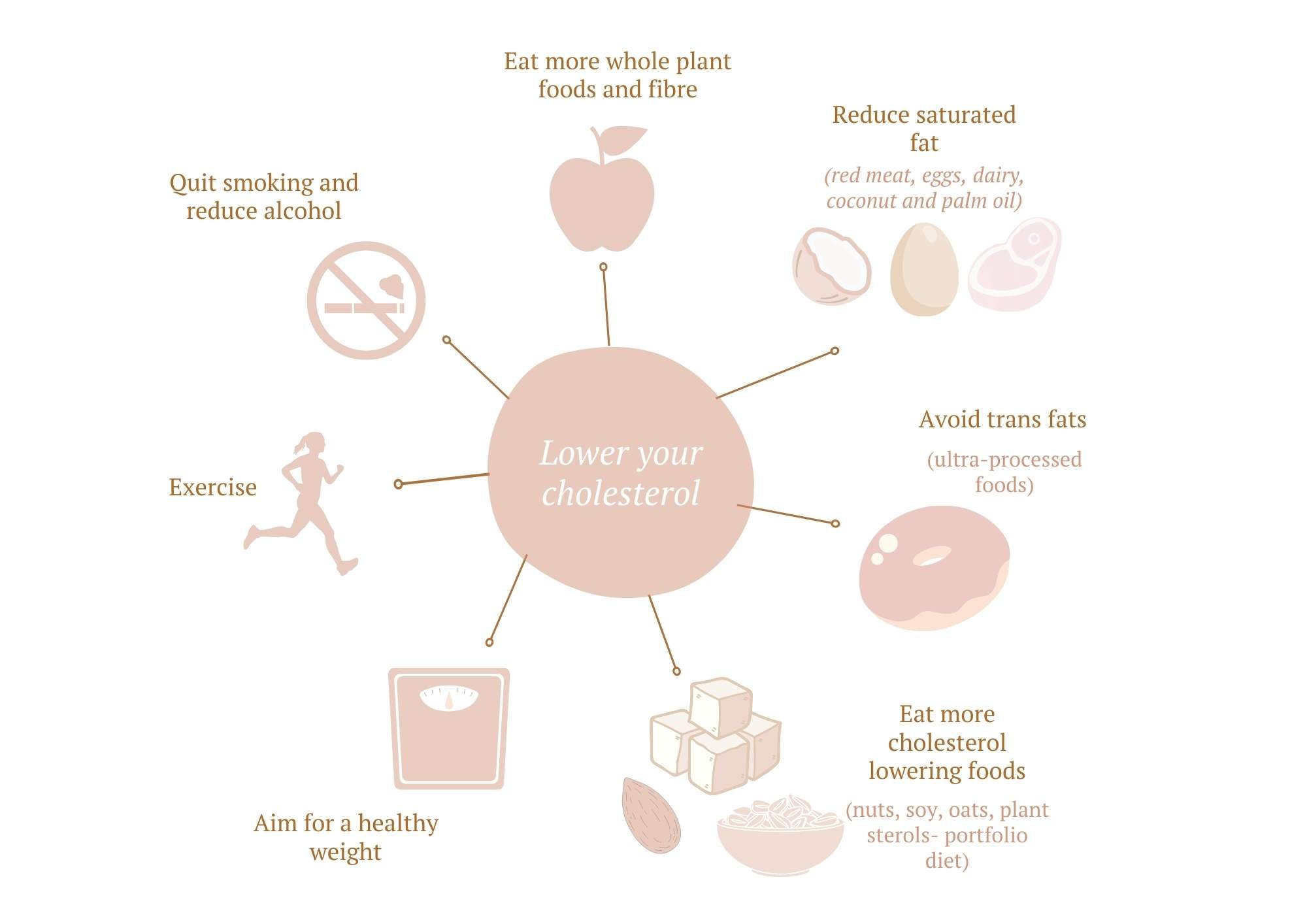
How Can You Improve Your Cholesterol Levels?
So now we’ve covered the basics of cholesterol, let’s dive into what YOU can do to help your cholesterol levels!
Lifestyle medicine is key, with diet playing the most significant role, complemented by exercise. The goal is to:
- Lower LDL cholesterol.
- Increase HDL cholesterol.
- Improve triglyceride:HDL ratio
- Reduce inflammation.
Let’s break it down, and look at ways to tackle each of these individually (although we’ll give you a sneaky tip – healthy lifestyle habits improve all of these at once!)
Eat To Reduce Your LDL
LDL levels are heavily influenced by the types of fats and cholesterol in your diet. The primary contributors are:
- Saturated fats.
- Trans fats.
- Dietary cholesterol.
Saturated fat is the first piece of the puzzle, it’s found in:
- Fatty meats (e.g., red meat).
- Full-fat dairy products.
- Eggs.
For every 1% of your energy intake that comes from saturated fat, your LDL will increase by 0.02–0.04 mmol/L!!
This means the lower you can keep your saturated fat intake, the lower your LDL cholesterol will be.
Key tips:
- Plants naturally contain little to no saturated fat (except tropical oils like coconut and palm oil).
- Shifting toward more whole plant foods and fewer animal products lowers LDL cholesterol.
Dietary cholesterol comes next, foods high in cholesterol include:
- Egg yolks.
- Shrimp.
- Beef, pork, and poultry.
- Cheese and butter.
Impact on LDL:
While dietary cholesterol raises LDL, its effect is less significant than that of saturated fat.
Remember: Your body produces all the cholesterol it needs, so consuming dietary cholesterol isn’t necessary.
Trans fats are the third (and lesser known) piece of the LDL puzzles, these are artificially created fats found in:
- Processed foods (look for “partially hydrogenated oils” on labels).
- Small amounts in meat and dairy.
Trans fats increase LDL and decrease HDL, they’re also highly inflammatory and harmful for heart health – which is why they are banned in many countries, but can still sneak into many processed foods!
Key tip: Avoid trans fats entirely—they’re unnecessary and banned in many countries due to their link to heart disease.

STEPS YOU CAN TAKE TO LOWER YOUR LDL CHOLESTEROL
To lower your LDL cholesterol naturally, there are two main strategies you can use – reducing intake of foods that INCREASE LDL, and increase your intake of foods that REDUCE LDL. Let’s break this down further..
REDUCE OR AVOID FOODS THAT INCREASE LDL:
- Avoid trans fats: Steer clear of processed foods containing partially hydrogenated oils.
- Limit saturated fats: Reduce intake of tropical oils, fatty meats, butter, cream, and regular cheese.
- Choose healthy fats:
- Monounsaturated fats: Extra-virgin olive oil.
- Polyunsaturated fats: Non-tropical vegetable oils (e.g., sunflower, flaxseed).
- These fats can reduce LDL and increase HDL.
- Limit saturated fat intake to:
- <10% of your total calories.
- <7% if your cholesterol is already high.
BOOST YOUR INTAKE OF FOODS THAT REDUCE LDL:
In addition to avoiding foods that raise LDL cholesterol, you can actively reduce LDL levels by incorporating specific cholesterol-lowering foods into your diet.
One of the simplest and most effective steps is to increase your soluble fiber intake. Soluble fiber, found exclusively in plant-based foods, can significantly lower cholesterol levels. Incorporating fruits, vegetables, nuts, seeds, legumes, and whole grains daily not only improves cholesterol but also supports overall heart health.
While fiber supplements are an option, consuming whole foods is always the better choice when possible.
Try The Portfolio Diet
There are also certain foods specifically shown to lower cholesterol. These are included in a dietary pattern called the ‘Portfolio diet’, often used to target high LDL levels. In fact following a Portfolio diet, can potentially lower LDL cholesterol by up to 30 %!! (Jenkins et al., 2003)
Key Portfolio Diet Components
Each day, aim for:
- Soy protein: 50 grams (from sources like tofu, edamame, and miso).
- Plant sterols: 2 grams (found in fortified foods or naturally in small amounts in plants).
- Nuts: 45 grams (about one handful or 23 almonds).
- Soluble fiber: 18 grams (from oats, barley, legumes, and other whole grains).
Each food has an additive effect, so every step you take counts.

How To Lower Triglycerides
While the focus for cholesterol lowering is usually on LDL cholesterol, triglycerides are important too!
High triglycerides are often a marker of insulin resistance, as well as of fatty liver disease and visceral fat, where excess harmful fat is stored in the liver. and internal organs. This fat is highly inflammatory, and if left unaddressed, can progress to more serious conditions.
Fortunately, high triglyceride levels (and visceral fat) are incredibly responsive to simple diet and lifestyle changes!
Here are some effective ways to reduce triglyceride levels and reduce visceral fat and fat in your liver:
- Stay Active: Regular exercise helps burn calories and improves fat metabolism.
- Avoid Overeating: Focus on balanced portions.
- Reduce Simple Carbs: Limit refined carbs, processed foods, and added sugars. This includes liquid sugars like soft drinks and fruit juices!
- Balance Your Plate: Aim for around half your diet to be non starchy veges; 25% to be lean protein (legumes, nuts, seeds, oily fish, chicken or eggs); and 25% to be complex (whole grain) carbohydrates.
- Be Mindful Of Alcohol: Alcohol is both toxic to your liver, and can also significantly increase triglyceride levels. Keep it to a minimum (or avoid it altogether) – ideally aiming for less than 2 standard drinks per week.
Together, these strategies not only lower triglycerides but also reduce the risk of prediabetes, diabetes, and fatty liver disease. Plus they’re great for overall health too!

THE POWER OF THE MEDITTERANEAN DIET
Still Doubting the Impact of Diet? Let’s Dive into the Evidence!
Two of the largest and most groundbreaking studies on diet and heart disease—the LYON Diet Heart Study and the PREDIMED Trial—provide compelling proof that what you eat can significantly affect your heart health.
The LYON Diet Heart Study
This study examined the effects of a Mediterranean-style diet on 500 individuals who had experienced their first heart attack. Participants were divided into two groups:
- Group 1: Continued their standard Western diet.
- Group 2: Adopted a plant-focused Mediterranean diet.
The Mediterranean diet emphasized:
- High intake: Fruits, vegetables, whole grains, potatoes, beans, nuts, and seeds.
- Primary fat source: Olive oil.
- Moderate amounts: Dairy, fish, and poultry.
- Minimal consumption: Eggs (0–4 weekly) and red meat.
Key Results (after 46 months):
- A 60% reduction in overall mortality.
- A 70% reduction in recurrent heart attacks.
The results were so striking that the trial was stopped early. Allowing the control group to continue a Western diet was deemed unethical, given their significantly higher risk of heart attacks and death.
Takeaway: No medication on the market offers such dramatic results as the Mediterranean diet.
The PREDIMED Study
This landmark study followed nearly 7,500 high-risk individuals to assess the impact of diet on heart disease prevention. Participants were divided into three groups:
- A Mediterranean diet supplemented with extra-virgin olive oil.
- A Mediterranean diet supplemented with mixed nuts.
- A standard low-fat diet.
Key Results (after almost 5 years):
- Both Mediterranean diet groups reduced their risk of heart attacks by 30% compared to people who followed a standard low fat diet—a reduction comparable to statin therapy.
Why This Matters
Both studies show that dietary changes alone can produce life-altering benefits for heart health. These results highlight the power of:
- High-fiber, plant-focused eating (as in the Mediterranean diet).
- Healthy fats from olive oil and nuts.
When combined with other heart-healthy habits—such as regular exercise, stress management, adequate sleep, reducing salt intake, and avoiding smoking—the benefits become even more profound.
Conclusion: The evidence is clear—diet is a cornerstone of heart health. It’s never too late to make changes, and the impact can be as significant as, or even greater than, many medications. You can use the graphic below to see how to follow a Mediterranean dietary pattern, like those used in the studies just mentioned.
Even if you’re prescribed statin medications, adopting heart-healthy dietary changes amplifies the benefits. A cholesterol-lowering diet doesn’t just help reduce LDL—it supports overall health and tackles multiple cardiovascular risk factors.
TO WRAP IT ALL UP
So to sum it all up, here are our top tips for improving cholesterol, so you can reduce your risk of heart disease, strokes, dementia, and other health issues:
- Eat whole foods, mostly plants.
- Boost your fiber intake by including fruits, vegetables, legumes, nuts, seeds, and whole grains daily.
- Focus on plant-based cholesterol-lowering foods like oats, soy, legumes, nuts, and plant sterols aka the Portfolio diet.
- Stay active—aim to move your body every day.
- Limit processed foods, added sugars, refined carbs, and alcohol—swap refined grains for whole grains.
- Adopt the Mediterranean diet pattern and use the wellness plate as your guide to balanced eating.
- Reduce saturated fats, especially from animal products, particularly if you have high cholesterol or other cardiovascular risks.
- Embrace anti-inflammatory habits:
- Follow an anti-inflammatory diet.
- Avoid cigarette smoke.
- Limit salt intake.
- Work towards a healthy weight range.
These are the same principles we recommend for overall good health—simple yet incredibly effective!
WANT TO LEARN MORE?
If this resonates with you, we dive deeper into these topics in our Reboot and Nutrition courses, designed to help you transform your health completely.
Need personalized advice? We offer virtual lifestyle medicine consultations across New Zealand (via secure telemedicine) too!. We’d love to work with you to create a tailored, evidence-based plan to optimize your cholesterol, heart health, and overall well-being.
👉 More details here —we can’t wait to help you take control of your health!
References:
Bruckert E, Rosenbaum D. Lowering LDL-cholesterol through diet: potential role in the statin era. Curr Opin Lipidol. 2011 Feb;22(1):43-8. doi: 10.1097/MOL.0b013e328340b8e7. PMID: 21233620.
Gigleux I, Jenkins DJ, Kendall CW, et al. Comparison of a dietary portfolio diet of cholesterol-lowering foods and a statin on LDL particle size phenotype in hypercholesterolaemic participants. Br J Nutr. 2007 Dec;98(6):1229-36. doi: 10.1017/S0007114507781461. Epub 2007 Jul 30. PMID: 17663803.
Bitzur R, Cohen H, Kamari Y, Harats D. [Phytosterols: another way to reduce LDL cholesterol levels]. Harefuah. 2013 Dec;152(12):729-31, 751. Hebrew. PMID: 24482998.
Ras RT, Geleijnse JM, Trautwein EA. LDL-cholesterol-lowering effect of plant sterols and stanols across different dose ranges: a meta-analysis of randomised controlled studies. Br J Nutr. 2014 Jul 28;112(2):214-9. doi: 10.1017/S0007114514000750. Epub 2014 Apr 29. PMID: 24780090; PMCID: PMC4071994.
Anderson KM, Castelli WP, Levy D. Cholesterol and mortality. 30 years of follow-up from the Framingham study. JAMA. 1987 Apr 24;257(16):2176-80. doi: 10.1001/jama.257.16.2176. PMID: 3560398.
Anderson, T. J., Gregoire, J., Pearson, G. J., Barry, A. R., et al. (2016). 2016 Canadian Cardiovascular Society Guidelines for the Management of Dyslipidemia for the Prevention of Cardiovascular Disease in the Adult. Can J Cardiol, 32(11), 1263-1282.
Asbaghi, O., Moodi, V., Hadi, A., Eslampour, E., Shirinbakhshmasoleh, M., et al. (2021). The effect of almond intake on lipid profile: a systematic review and meta-analysis of randomized controlled trials. Food Funct, 12(5), 1882-1896.
Basora, J., Munoz, M. A., Sorli, J. V., Martinez, J. A., Fito, M., Gea, A., . . . Investigators, P. S. (2018). Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N Engl J Med, 378(25), e34.
Blanco Mejia, S., Messina, M., Li, S. S., Viguiliouk, E., Chiavaroli, L., Khan, T. A., et al. (2019). A Meta-Analysis of 46 Studies Identified by the FDA Demonstrates that Soy Protein Decreases Circulating LDL and Total Cholesterol Concentrations in Adults. J Nutr, 149(6), 968-981.
Chiavaroli, L., Nishi, S. K., Khan, T. A., Braunstein, C. R et al (2018). Portfolio Dietary Pattern and Cardiovascular Disease: A Systematic Review and Meta-analysis of Controlled Trials. Prog Cardiovasc Dis,61(1), 43-53.
Chiavaroli, L., Viguiliouk, E., Nishi, S. K., Blanco Mejia, S., Rahelic, D et al. (2019). DASH Dietary Pattern and Cardiometabolic Outcomes: An Umbrella Review of Systematic Reviews and Meta-Analyses. Nutrients, 11(2).
de Souza, R. J., Mente, A., Maroleanu, A., Cozma, A. I., Ha, V., Kishibe, T., Uleryk, E., Budylowski, P., Schünemann, H., Beyene, J., & Anand, S. S. (2015). Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies. BMJ (Clinical research ed.), 351, h3978.
Estruch, R., Ros, E., Salas-Salvado, J., Covas, M. I., Corella, D., Aros, F., Gomez-Gracia, E., Ruiz-Gutierrez, V., et sl(2016a). The effect of oat beta-glucan on LDL-cholesterol, non-HDL-cholesterol and apoB for CVD risk reduction: a systematic review and meta-analysis of randomised-controlled trials. Br J Nutr, 116(8), 1369-1382.
Ho, H. V., Sievenpiper, J. L., Zurbau, A., Blanco Mejia, S., Jovanovski, E., Au-Yeung, F., Jenkins, A. L., & Vuksan, V. (2016b). A systematic review and meta-analysis of randomized controlled trials of the effect of barley beta-glucan on LDL-C, non-HDL-C and apoB for cardiovascular disease risk reduction(i-iv). Eur J Clin Nutr,70(11), 1239-1245.
Hooper, L., Martin, N., Jimoh, O. F., Kirk, C., Foster, E., & Abdelhamid, A. S. (2020). Reduction in saturated fat intake for cardiovascular disease. The Cochrane database of systematic reviews, 5(5), CD011737.
Jenkins D, et al. Effects of a dietary portfolio of cholesterol-lowering foods vs lovastatin on serum lipids and C-reactive protein. JAMA. 2003 Jul 23;290(4):502-10. doi: 10.1001/jama.290.4.502.
Martinez-Gonzalez, M. A., Gea, A., & Ruiz-Canela, M. (2019). The Mediterranean Diet and Cardiovascular Health. Circ Res, 124(5), 779-798.
Mazidi, M., Mikhailidis, D. P., Sattar, N., Toth, P. P., Judd, S., Blaha, M. J., Hernandez, A. V., Penson, P. E., Banach, M., & International Lipid Expert Panel (ILEP) & Lipid and Blood Pressure Meta-analysis Collaboration (LBPMC) Group (2020). Association of types of dietary fats and all-cause and cause-specific mortality: A prospective cohort study and meta-analysis of prospective studies with 1,164,029 participants. Clinical nutrition (Edinburgh, Scotland), 39(12), 3677–3686.
Pearson, G. J., Thanassoulis, G., Anderson, T. J., Barry, A. R., Couture, P., Dayan, N., Francis, G. A., et al(2021). 2021 Canadian Cardiovascular Society Guidelines for the Management of Dyslipidemia for the Prevention of Cardiovascular Disease in Adults. Can J Cardiol, 37(8), 1129-1150.
Quek, J., Lim, G., Lim, W. H., Ng, C. H., So, W. Z., Toh, J., Pan, X. H., Chin, Y. H., Muthiah, et al. (2021). The Association of Plant-Based Diet With Cardiovascular Disease and Mortality: A Meta-Analysis and Systematic Review of Prospect Cohort Studies. Front Cardiovasc Med, 8, 756810.
Schoeneck, M., & Iggman, D. (2021). The effects of foods on LDL cholesterol levels: A systematic review of the accumulated evidence from systematic reviews and meta-analyses of randomized controlled trials. Nutrition, metabolism, and cardiovascular diseases : NMCD, 31(5), 1325–1338.
Tokede, O. A., Onabanjo, T. A., Yansane, A., Gaziano, J. M., & Djousse, L. (2015). Soya products and serum lipids: a meta-analysis of randomised controlled trials. Br J Nutr, 114(6), 831-843.
Trautwein, E. A., Vermeer, M. A., Hiemstra, H., & Ras, R. T. (2018). LDL-Cholesterol Lowering of Plant Sterols and Stanols-Which Factors Infl
uence Their Efficacy? Nutrients, 10(9).
Vincent, M. J., Allen, B., Palacios, O. M., Haber, L. T., & Maki, K. C. (2019). Meta-regression analysis of the effects of dietary cholesterol intake on LDL and HDL cholesterol. The American journal of clinical nutrition, 109(1), 7–16.
Zhuang, P., Wu, F., Mao, L., Zhu, F., Zhang, Y., Chen, X., Jiao, J., & Zhang, Y. (2021). Egg and cholesterol consumption and mortality from cardiovascular and different causes in the United States: A population-based cohort study. PLoS medicine, 18(2), e1003508.
Bittner V, Johnson BD, Zineh I, Rogers WJ, Vido D, Marroquin OC, Bairey-Merz CN, Sopko G. The triglyceride/high-density lipoprotein cholesterol ratio predicts all-cause mortality in women with suspected myocardial ischemia: a report from the Women’s Ischemia Syndrome Evaluation (WISE). Am Heart J. 2009 Mar;157(3):548-55. doi: 10.1016/j.ahj.2008.11.014. PMID: 19249427; PMCID: PMC2677623.
Summary of evidence for lifestyle strategies to reduce cholesterol
https://academic.oup.com/eurheartj/article/41/1/111/5556353?login=false (European lipid guidelines)



