
Your Holistic Guide to Perimenopause and Menopause
Are you in your late 30s, 40s, or 50s and feeling like your body—and life—just got a whole lot more complicated?
You’re not alone. And chances are, your hormones have something to do with it.
Perimenopause and menopause bring profound changes to a woman’s body, yet they’re rarely discussed openly. As a result, many women struggle in silence for years before realizing what’s happening.
During this transition, key hormones like estrogen and progesterone fluctuate massively before eventually declining, marking the end of menstrual cycles and fertility. The experience is unique for every woman—some breeze through it, while others face challenging symptoms. But one thing is certain: perimenopause is a natural phase of life, not an illness.
What’s fascinating is that humans are one of the few species where females live long past their reproductive years. Research suggests that postmenopausal women have played a crucial role in human survival, with their wisdom and experience benefiting families and communities. Historically, families with grandmothers present had better nutrition and higher child survival rates—a testament to their importance.
Yet in today’s fast-paced world, many women juggle careers, family responsibilities, and personal well-being during this hormonal shift, making it a particularly demanding time. Studies show menopause can impact work productivity, job satisfaction, and even career progression, making it more than just a personal issue—it’s a societal one too.
The good news? Knowledge is power. By understanding and embracing this transition, women can take charge of their health, well-being, and future. So let’s start the conversation—because an empowered menopause is a healthier, happier one!
Understanding Perimenopause and Menopause
Before we dive in, let’s clarify what perimenopause and menopause actually mean.
Perimenopause is the transition phase leading up to menopause, during which hormone levels—especially estrogen and progesterone—fluctuate significantly and gradually decline. While ovulation and menstruation still occur, periods may become irregular, heavier, or lighter. Many women experience symptoms during this stage due to shifting hormone levels, and this phase can last for several years.
Menopause officially begins when the ovaries stop producing hormones and a woman has gone 12 consecutive months without a period. If periods have stopped due to medication or surgery (such as a hysterectomy), menopause can be diagnosed through blood tests measuring FSH (follicle-stimulating hormone), LH (luteinising hormone). and estradiol levels.
A common misconception is that hormonal symptoms only happen after periods stop, and that they are limited to hot flashes, night sweats, and vaginal dryness. However, perimenopause can be just as challenging—if not more so—due to unpredictable hormonal swings. In reality, symptoms of both perimenopause and menopause are incredibly diverse and may include:
- Mood swings, anxiety, and depression
- Migraines and heart palpitations
- Joint pain and muscle stiffness
- Brain fog and memory issues
- Poor sleep and chronic fatigue
- Weight gain and changes in metabolism
- Hair thinning, dry skin, and brittle nails
- Increased cholesterol and blood sugar levels
It may seem surprising that perimenopause and menopause affects so many aspects of health, but it makes perfect sense—estrogen receptors exist in nearly every cell of a woman’s body! This is why hormonal changes can impact everything from brain function to heart health.
Understanding these shifts is the first step in managing them, so let’s explore how you can navigate this transition with confidence and well-being.
Phases of perimenopause
Very Early Perimenopause (Mid to Late 30s)
During this stage, your menstrual cycle remains regular, but you may start noticing subtle changes—such as worsening PMS symptoms. Many women don’t realize that these mild shifts are actually the first signs of hormonal changes associated with perimenopause.
Early Perimenopause
As perimenopause progresses, progesterone levels begin to decline, while estrogen remains relatively high. This hormonal imbalance happens in part, because ovulation (the release of an egg) becomes less frequent, leading to lower progesterone production. Supporting progesterone levels during early perimenopause can help with symptom management.
You might notice:
- A slightly shorter menstrual cycle (by 1–2 days)
- Occasional missed periods (1–2 times per year)
- More intense PMS, mood swings, and irritability
- Heavier periods
- Increased anxiety and brain fog
- Breast pain
- Insomnia
- Migraines.
These changes can be subtle at first, but they mark the beginning of a transition that will continue over the next several years. Understanding these early signs can help you take proactive steps to support your hormonal health and well-being.
Late perimenopause and beyond
As perimenopause progresses, estrogen levels begin to decline alongside progesterone. This is when menstrual cycles become more irregular—periods may become lighter, spaced further apart, or skipped entirely.
With lower estrogen, symptoms like hot flashes, night sweats, and vaginal dryness often become more noticeable. Once a woman has gone 12 consecutive months without a period, she is officially in menopause. From that point forward, she is considered postmenopausal.
Supporting both estrogen and progesterone during this transition can be key to managing symptoms and maintaining overall well-being. Understanding these changes can help you make informed choices to feel your best through every stage of menopause and beyond.

The Hidden Impact of Perimenopause and Menopause on Mood and Well-Being
Perimenopause can bring more than just physical changes—it can also trigger significant mood swings, sleep disturbances, and even new-onset anxiety or depression.
Because these symptoms can mimic stress, mental health conditions, or even chronic fatigue and pain disorders, they’re often misdiagnosed. If hormonal changes aren’t considered, women may be left struggling without the right support.
While stress and other factors can certainly play a role, for many women, fluctuating hormones are the primary driver of these symptoms. Addressing the hormonal imbalance itself as well as taking a holistic approach to supporting body and mind—rather than just managing the symptoms—can often lead to far better outcomes.
Menopause also comes with a wide range of symptoms, some well-known, like hot flashes and night sweats, and others less obvious, such as:
- Muscle pain and weakness
- Heart palpitations
- Migraines and headaches
- Brain fog and memory issues
These changes can feel overwhelming, but recognizing the hormonal connection is the first step toward finding effective relief.
Menopause and Long-Term Health: What You Need to Know
Menopause isn’t just about the end of periods either—it also increases the risk of several health conditions due to the loss of estrogen’s protective effects. These include:
- Heart disease
- Dementia and cognitive decline
- Type 2 diabetes
- High blood pressure
- Osteoporosis (weakened bones)
- Depression and mood disorders
That’s why focusing on preventive health strategies—especially through lifestyle choices—is a key part of staying strong and healthy during and after menopause.
Interestingly, even after the ovaries stop producing estrogen, a small amount is still made by fat cells. This may be one reason why weight gain is common during menopause—particularly around the hips and thighs, where some fat storage is actually protective and completely normal.
However, excess weight gain around the abdomen (visceral fat) can increase the risk of metabolic issues like heart disease and diabetes, making it important to find a healthy balance.
The good news? There are many ways to support your body through menopause and set yourself up for lifelong well-being.
Let’s dive into what you can do to optimize your health, feel your best, and truly thrive through this transition!
A Holistic Approach to Perimenopause and Menopause
Perimenopause and menopause are more than just a collection of symptoms—they represent a profound shift in your body, mind, and overall well-being. A holistic approach acknowledges this by focusing on nourishing the whole person through:
- Regular movement to support metabolism, bone health, and mood
- Balanced nutrition to provide essential nutrients and hormonal support
- Quality sleep to aid in recovery and energy levels
- Mindfulness and stress management to regulate the nervous system
- Meaningful relationships to enhance emotional resilience
While genetics play a role in when and how menopause unfolds, your overall health leading up to perimenopause can have a major impact on your experience. Establishing strong health foundations early on can help ease symptoms and reduce the risk of chronic conditions later in life.
This stage of life is also a critical window for long-term health. Hormonal shifts can trigger new health concerns or worsen existing ones, making it essential to take a comprehensive, proactive approach. This includes:
- Metabolic health (blood sugar, cholesterol, and cardiovascular function)
- Bone health (preventing osteoporosis)
- Gut health (nutrient absorption and inflammation control)
- Nervous system regulation (mood, stress, and cognitive function)
- Identifying imbalances such as nutrient deficiencies, or other hormonal conditions such as thyroid disorders or insulin resistance
By addressing these factors holistically, you can navigate perimenopause with confidence while laying the foundation for vibrant health in the years to come.

The Vital Role of Nutrition in Perimenopause & Menopause
What you eat can have a profound impact on how you experience perimenopause and menopause. A well-balanced diet can help reduce symptoms by up to 30% and lower the risk of long-term health issues.
One of the most researched and recommended approaches is a Mediterranean-style, anti-inflammatory, whole-food, plant-rich diet. This way of eating supports:
✔️ Heart, brain, and bone health
✔️ Hormonal balance and metabolism
✔️ Gut health and inflammation control
✔️ Stronger immune function
A 2022 study found that following a Mediterranean diet can significantly reduce the severity of menopausal and psychological symptoms, particularly in individuals with a higher BMI. The most beneficial components were increased intake of legumes and extra-virgin olive oil.
Another study linked higher consumption of vegetables, whole grains, and unprocessed foods to lower intensity of psychological symptoms, sleep disturbances, and vasomotor, urogenital, and somatic symptoms. In contrast, processed foods, saturated fats, sugars, and caffeine were associated with worsening symptom intensity.
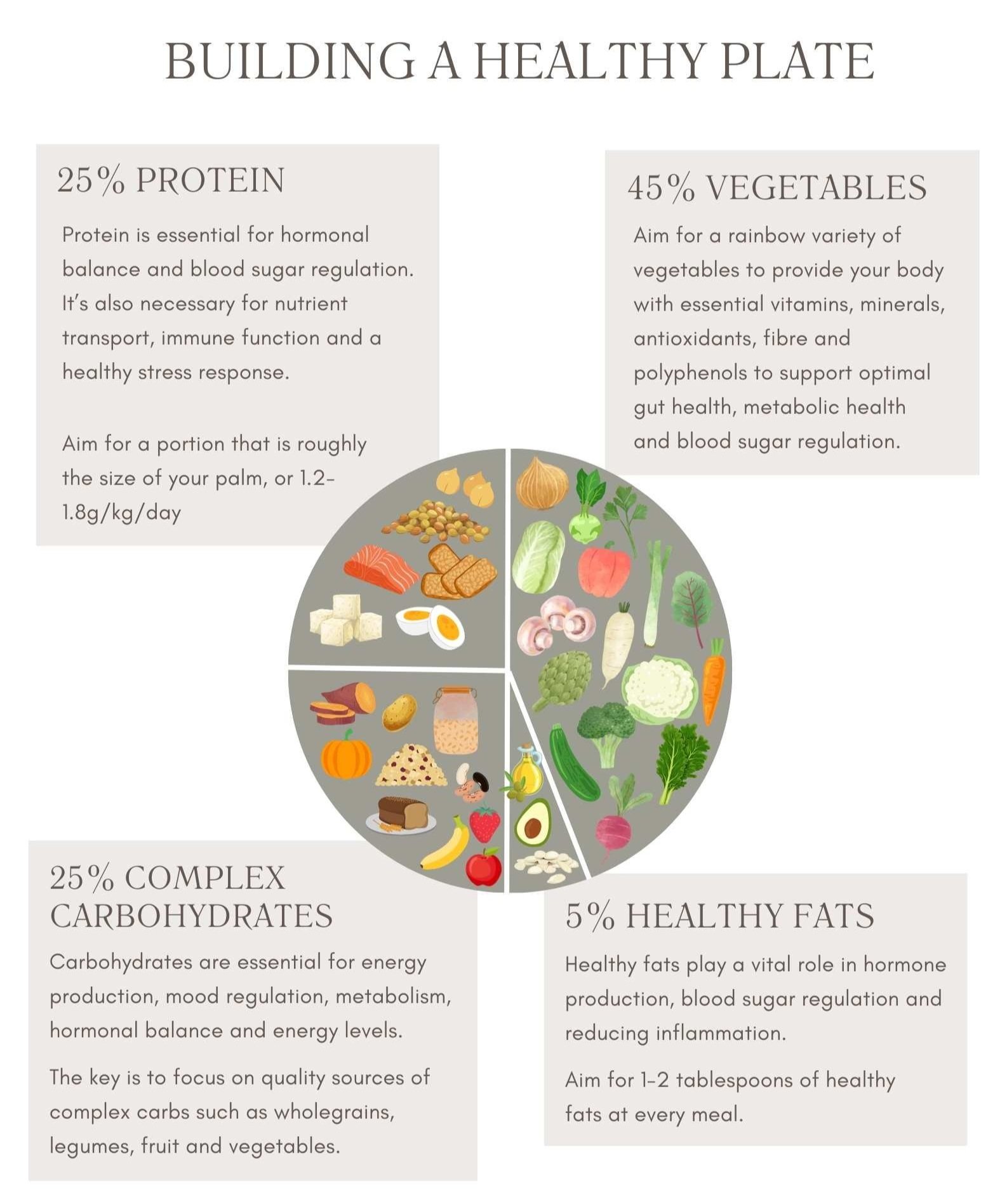
General Nutrition Tips for Perimenopause & Menopause
A balanced diet plays a crucial role in managing menopausal symptoms and supporting long-term health. Choosing whole grains over refined carbs helps maintain stable energy levels and supports metabolic health. Limiting ultra-processed foods and added sugars can reduce inflammation and prevent blood sugar spikes.
Instead of saturated fats found in fatty meats and full-fat dairy, opt for healthy unsaturated fats like seeds, nuts, avocado, and olive oil, which promote heart and hormone health. Keeping total fat intake around 30% of daily calories may also help reduce hot flashes and night sweats.
Including legumes, seeds, and nuts daily provides fiber for gut health and phytoestrogens that support hormone balance. Aiming for five or more servings of colorful vegetables each day, with an emphasis on non-starchy, above-ground varieties, along with at least two servings of fruit, helps supply essential vitamins and minerals.
Leafy greens should be a daily staple, as they are packed with anti-inflammatory compounds, calcium, vitamin K, B vitamins, and magnesium, all of which support mood, sleep, and bone health. Similarly, cruciferous vegetables like broccoli, kale, cauliflower, Brussels sprouts, and cabbage aid in hormone balance, liver detoxification, and cancer protection.
Ensuring adequate omega-3 intake from fish, flaxseeds, walnuts, chia seeds, and hemp hearts is beneficial for brain, heart, and immune function.
Prioritizing protein at each meal helps balance blood sugar and supports muscle and bone health, with perimenopausal and menopausal women needing around 1.2–1.6g/kg of protein per day, increasing after age 65 to prevent muscle loss. While plant-based proteins from legumes, nuts, seeds, and whole grains are highly recommended, incorporating fish, chicken, and eggs in moderation can be beneficial. Red meat consumption should be limited to 300g per week for optimal health.
Key Micronutrients To Know About
✔️ B12, Iron, Folate & Iodine – Essential for energy, mental health, and thyroid function (check levels with a blood test if unsure)
✔️ Calcium (1200mg/day) – Crucial for bone health, found in tofu, leafy greens, seeds, legumes, and dairy
✔️ Vitamin K – Supports bone, brain, and heart health, found in dark leafy greens
✔️ Vitamin D – Critical for bone health, mood, and immune function (sun exposure or supplementation, especially in winter)
Gut Health & Hormonal Balance
A healthy gut is essential for hormonal balance, metabolism, mood, inflammation control, and overall health.
To support gut health:
✔️ Increase fiber intake (at least 30g/day from diverse plant foods)
✔️ Eat probiotic-rich foods (fermented foods like yogurt, kimchi, sauerkraut, kefir)
✔️ Aim for 30 different plant foods per week to nourish gut bacteria
New research suggests that gut bacteria play a crucial role in hormone metabolism—a well-balanced microbiome can help reduce menopausal symptoms, improve mood, and support overall health.
The Power of Phytoestrogens
Phytoestrogens are plant compounds that mimic estrogen and help balance hormones. They are found in:
✔️ Soy (tofu, tempeh, edamame, soy milk)
✔️ Flaxseeds, sesame seeds, chickpeas, whole grains, berries, barley, and tea
These compounds act as Selective Estrogen Receptor Modulators (SERMs)—providing pro-estrogenic effects where needed (reducing menopause symptoms) and anti-estrogenic effects where excess estrogen is harmful (reducing risks of fibroids, breast and endometrial cancers).
Studies show soy consumption is linked to a lower risk of breast cancer and improved menopausal symptoms, including hot flashes, cognitive health, and sleep quality. Whole and minimally processed soy products are best.
Time-Restricted Eating (TRE)
Emerging research suggests eating within a 10–12 hour window can support weight management, blood sugar, and metabolic health. However, extended fasting is not recommended for women with a history of eating disorders or malnutrition.
The Takeaway
To thrive through perimenopause and beyond, focus on:
- Whole, plant-rich foods
- A variety of colors & nutrients
- Balanced protein & healthy fats
- Optimized gut & hormone health
Your body—and your future self—will thank you!

Why You Should Limit Alcohol, Caffeine, and Tobacco exposure
Alcohol is not always a popular topic, but it’s particularly important during perimenopause and menopause, as it increases the risk of many cancers (especially breast cancer), and can negatively impact heart and brain health as well as sleep and mood. It can also worsen osteoporosis, and is a common hidden cause of weight gain! Advice is to drink as little as possible, and if you do choose to drink, limit to no more than 10 units per week.
Caffeine in itself is fine, but it may worsen hot flushes and poor sleep in some women, so it can be worth considering cutting it out or switching to decaffeinated coffee if you have these symptoms.
Smoking should be avoided completely if possible, as it tends to worsen menopause symptoms (especially hot flushes), as well as increasing the risk of heart disease, dementia, and osteoporosis.
If you do smoke, quitting (or cutting down as much as possible if quitting is not an option) it’s strongly recommended, and menopause is a great reason to do so! If you struggle with this there are lots of great options to help you quit – talk to your doctor or a quit smoking provider for more details.

Movement for A Healthier Transition
The benefits of building and maintaining muscle mass during perimenopause cannot be overstated. As oestrogen levels drop throughout the transition, movement can be a vital player to help combat the health effects of this change. Exercise supports metabolic health and body composition, blood sugar balance, stress reduction and blood circulation to your reproductive system. It also helps sleep, mood, energy, and bone health, and can even reduce hot flushes.
If you’re just starting to incorporate more movement into your daily routine, then any physical activity is better than none. Ideally, you want to aim for at least 20-30 minutes of moderate-intensity exercise every day. This includes anything that increases your heart rate and breathing, but still allows you to carry on a conversation. This could include a fast-paced walk, bike ride, swim, pilates, climbing stairs, or even household chores like gardening or sweeping.
It’s also recommended that you do muscle-strengthening activity/resistance training at least two or more days every week. This includes bodyweight exercises such as push-ups, lunges and squats, using weights to perform exercises, pilates, certain types of yoga focused on building strength and heavy gardening work like digging or shovelling.
Strength training helps to build muscle mass as the exercise that moves muscle against resistance, stimulating the muscle to grow stronger. It’s particularly vital in perimenopause and beyond, as women progressively lose muscle mass from age 40, and can lose up to 10% of muscle mass in the perimenopausal transition!
Preserving muscle is key for immune health, metabolic health, and bone health, as the process of muscle loss (sarcopenia, which also occurs in men) is linked with poorer long-term health in many areas as well as reduced life expectancy.
Many women also enjoy more intense exercise such as HIIT or running, which can lead to greater benefits for cardiovascular health, insulin sensitivity and body composition. Be careful not to overdo it, as too much high-intensity exercise is a stressor on the body. Listen to your body and avoid this type of exercise when you are highly stressed, unwell or feeling depleted.
Very short HIIT sequences (30s) with rest breaks (1-2min) in between can create an ideal balance – getting your heart rate up but allowing recovery in between to avoid elevated cortisol.
How to incorporate more movement into your daily life:
- Set small, achievable goals that you can sustain over time.
- Try habit stacking where you take an already established habit and add some exercise. For example 10 squats every time you brush your teeth.
- Try to sit less and move more. For every hour that you sit down, get up and do 5 minutes of walking or stretching.
- Exercise with a friend or partner, or join a fitness class. This can help keep you accountable and motivated.
We take a detailed look at physical movement and how it affects our health, as well as how to make sure you’re doing the right exercise – plus online resistance training, balance, and flexibility workouts to help you get moving – in our Reboot and Boost your Activity courses!.

Sleep
Disrupted sleep is the second most common perimenopause symptom after hot flashes. There are many factors that can contribute to poor sleep during this time including hormonal fluctuations, night sweats, disrupted circadian rhythm and stress.
During sleep, your body engages in vital restorative processes, repairing and rejuvenating tissues, cleansing and removing waste products and toxins, balancing hormones and recalibrating your nervous system.
Skipping sleep compromises your body’s ability to heal and recharge. This can lead to imbalances that manifest as fatigue, irritability, mood changes, impaired mental clarity, metabolic disturbance, impaired stress resilience, a weakened immune system and even an increased risk of chronic health conditions. Prioritising quality sleep can help to improve vitality, resilience and overall health.
Our sleep-wake cycle is regulated by a delicate balance of chemicals and our internal body clock known as our circadian hythm. When daylight diminishes, our brain releases melatonin, which signals to our body that it’s time to wind down and prepare for sleep. Another major player is a chemical called adenosine, which builds up in our brain throughout the day as we engage in activities. As levels of adenosine rise, so does our sleep drive, which eventually leads to drowsiness and the need for restorative sleep.
Sleep Hygiene Practices
Establish a consistent sleep schedule: A consistent sleep schedule is important for regulating your circadian rhythm. It trains your body to release sleep-promoting chemicals at the right time to promote restful sleep. Try to go to bed and wake up at the same time every day, even on weekends and resist the urge to hit the snooze button.
Create a relaxing bedtime routine: Winding down before bed signals to your body that it’s time to sleep. Try reading a book, having a bath, gentle yoga or listening to calm music.
Limit caffeine: Caffeine keeps you alert by blocking adenosine receptors in the brain. This makes it more difficult to fall asleep and reduces the overall quality of sleep. I recommend avoiding coffee, tea and other sources of caffeine like dark chocolate at least 4-6 hours before bed.
Limit alcohol: Alcohol can initially make you drowsy by stimulating GABA, a calming neurotransmitter in your brain. However as your body processes the alcohol while you’re asleep, it interferes with other sleep hormones, leading to fragmented and less restorative sleep. So whilst it’s tempting to have a glass of wine before bed, this can affect your quality of sleep during the night and make you feel unrefreshed when you wake up. It’s best to avoid alcohol 3-4 hours before bedtime.
Limit bright lights and screens: Blue light emitted from screens and bright lights can signal to your brain that it’s daytime and suppress melatonin production. Use soft, warm lighting at night and limit screens 1-2 hours before bed. You can also use blue-light-blocking apps like f.lux or tinted blue-light glasses.
Exercise and natural light: Exercise increases adenosine levels and helps to regulate your circadian rhythm. Likewise, natural light exposure, especially in the morning, helps to regulate your body’s sleep-wake cycle, making it easier to fall asleep and wake up refreshed.
Natural remedies: Herbal teas like chamomile and passionflower as well as magnesium oil applied topically can also help with relaxation and sleep. Supplementing magnesium or melatonin can also be effective (melatonin is prescription only in New Zealand)
HRT: HRT can be incredibly effective for helping restore healthy sleep, so if you are struggling with poor sleep despite these tips, consider talking to your doctor about whether this is right for you.
You can learn more about how sleep works, it’s effects on health, and how to improve it in depth in our Reboot and Restore your Sleep courses. Or for some simple tips check out our sleep article.

The Impact of Perimenopause and Menopause on Mood and Stress
In this day and age, it’s rare to find anyone who isn’t stressed. But the harsh reality is what’s common isn’t necessarily normal. Perimenopause can be a particularly stressful time, so it’s important to build a support team around you and develop healthy coping strategies to bring your nervous system back into balance. It’s also important to familiarise yourself with different sources of stress that you may not be aware of, and minimise these as much as possible.
Stress and mood are influenced strongly by hormonal changes in perimenopause, as oestrogen helps to regulate cortisol (stress hormone) production, meaning the drop in oestrogen can end up in women operating in a ‘higher cortisol’ state, where the nervous system is activated. Progesterone also has a calming effect on the nervous system, so a lack of this adds to stress and anxiety levels.
This can lead to feelings of irritability, being ‘on edge’ and anxious, and having a shorter fuse than normal, which can come out of the blue for some women. Pre-existing issues such as PMS, ADHD, PMDD, anxiety and depression can all be amplified.
Stress can come from a number of different sources, not just those we instantly think of as stressful. These can include:
Psychological stressors: self-criticism, lack of boundaries, toxic relationships, multitasking, perfectionism, comparison to others, trauma.
Physical stressors: skipping meals, too much or too little exercise, inflammation, poor gut health, nutrient deficiencies, poor sleep.
Environmental stressors: Excess artificial light esp. at night, technology overload, environmental toxins, doom scrolling, exposure to negative news and media, work demands, financial difficulties.
How to Manage Stress in Perimenopause and Menopause
Removing sources of stress
Start by making a list of things that cause you stress. This can include external factors like financial issues and work deadlines or internal factors like self-criticism. Categorise your stressors into things you can control and things you can’t. Make a plan for the ones that you can control. This could mean changing your routine, setting boundaries or seeking the help of a therapist.
This may mean saying ‘no’ more often, cutting back on work responsibilities if this is an option, delegating more and sharing the load, and getting rid of unnecessary commitments (as well as not trying to do too much!)
Even practical things like meal delivery boxes and hiring a cleaner (if this is financially an option), or sharing transport/after-school care of your children with other parents can make a big difference. Getting other household members on board to share the load is also a great idea if possible.
Regulating your nervous system
To support optimal nervous system function it’s important to find mindfulness activities that work for you and practice them regularly. This can include deep breathing, meditation, yoga, qi gong, journalling, getting out in nature and even gentle exercise. Bringing your attention to the present moment helps to calm your body and reduce stress hormones.
Be kind to yourself, and ideally try prioritise time for yourself to ‘refill’ your bucket’, just as you do daily responsibilities and chores.
Supporting your body
To support your body during times of stress, try to eat to keep blood sugar levels and energy balanced and even, aiming for regular wholegrain carbs/lower sugar meals, adequate protein, and lots of fibre.These all help to reduce the effects of stress on the body and mind, as blood sugar ‘spikes and crashes’ from high sugar/refined carb/low protein meals will often worsen food cravings and fatigue. It’s extremely common to crave sugar and ‘white’carbs when stressed or tired, as this is the bodies way of trying to get a quick energy fix, yet it actually tends to make symptoms worse overall – understanding why cravings are occurring can be helpful.
Professional support
There are many health professionals out there that can help you to manage your mental health during your perimenopause journey. Your doctor can offer a referral to a counsellor or psychologist and n integrative practitioner can offer personalised herbal, nutritional, dietary and lifestyle support. There are also hotlines and resources such as the 1737 helpline https://1737.org.nz/ or Lifeline https://www.lifeline.org.nz/
Recognise your body and mind are going through a large period of change, that although natural, may require you to slow things down and listen to your body more. This can often have a silver lining, as you become more aware of looking after yourself and investing in your health – which pays off massively in the long term!.
We take a deep dive into how stress works, how the mind and body are connected, and practical evidence based ways to reduce stress (and improve your ability to manage it) in our Reboot and Take control of your Stress courses.
Final Words
Navigating perimenopause and menopause can be overwhelming experiences, not just due to the physical symptoms but also the emotional impact that this transitional phase can bring. It’s important to be gentle with yourself, build a supportive network around you and prioritise self-love and self-care.
Remember that nobody is perfect and making significant diet and lifestyle changes takes time. Go at your own pace and set small, achievable goals.
While this blog covers lifestyle and diet, body-identical HRT can also be a helpful tool for many women, particularly if symptoms are impacting significantly on quality of life. Talk to your practitioner if you would like to discuss this and see if it is right for you – and don’t be afraid to seek help if you are struggling.
We prescribe them regularly alongside lifestyle strategies, and like many other medicines, can be a useful tool to have in your toolbox – lifestyle and medication can go hand in hand if needed!
The Japanese word for menopause is konenki, which means renewal years or energy – we love this phrase, as it changes our perception of menopause from a time of loss or negativity, to a time of new beginnings!!!
If you’ve enjoyed this article, please share it with others who might find it helpful, and follow us on social media for lots more tips and articles, we’d love to help you on your journey to better well-being ❤️
REFERENCES :
Safabakhsh M, Siassi F, Koohdani F, Qorbani M, Khosravi S, Abshirini M, Aslani Z, Khajehnasiri F, Sotoudeh G. Higher intakes of fruits and vegetables are related to fewer menopausal symptoms: a cross-sectional study. Menopause. 2020 May;27(5):593-604. doi: 10.1097/GME.0000000000001511. PMID: 32068682.
Shifren JL, Gass ML, NAMS Recommendations for Clinical Care of Midlife Women Working Group. The North American Menopause Society recommendations for clinical care of midlife women. Menopause. 2014;21(10):1038-62. [PMID:25225714]
Bolland MJ, Leung W, Tai V, et al. Calcium intake and risk of fracture: systematic review. BMJ . 2015;351-365.
Tai V, Leung W, Grey A, Reid IR, Bolland MJ. Calcium intake and bone mineral density: systematic review and meta-analysis. BMJ . 2015;351-365.
Pludowski P, Holick MF, Pilz S, et al. Vitamin D effects on musculoskeletal health, immunity, autoimmunity, cardiovascular disease, cancer, fertility, pregnancy, dementia and mortality-a review of recent evidence. Autoimmun Rev. 2013;12(10):976-89. [PMID:23542507]
Kim JK, Park SU. Current potential health benefits of sulforaphane. EXCLI J. 2016. 15:5. 571-577.
Ruan, X., Seeger, H., Wallwiener, D. et al.. The ratio of the estradiol metabolites 2-hydroxyestrone (2-OHE1) and 16α-hydroxyestrone (16-OHE1) may predict breast cancer risk in postmenopausal but not in premenopausal women: two case–control studies. Arch Gynecol Obstet. 2015. 291. 1141-1146.
Bahadoran Z, Tohidi M, Nazeri P, Mehran M, Azizi F, Mirmiran P.. Effect of broccoli sprouts on insulin resistance in type 2 diabetic patients: a randomized double-blind clinical trial.. Int J Food Sci Nutr. 2012. 63(7). 767-771.
Axelsson AS, Tubbs E, Mecham B, Chacko S, Nenonen HA, Tang Y, Fahey JW, Derry JM, Wollheim CB, Wierup N, Haymond MW, Friend SH, Mulder H, Rosengren AH. Sulforaphane reduces hepatic glucose production and improves glucose control in patients with type 2 diabetes. Science: Translational Medicine. 2017. 9.
Connolly EL, Sim M, Travica N, Marx W, Beasy G, Lynch GS, Bondonno CP, Lewis JR, Hodgson JM and Blekkenhorst LC (2021). Glucosinolates From Cruciferous Vegetables and Their Potential Role in Chronic Disease: Investigating the Preclinical and Clinical Evidence. Front. Pharmacol. 2021. 12. 767975.
Tortorella SM, Royce SG, Licciardi PV, Karagiannis TC. Dietary Sulforaphane in Cancer Chemoprevention: The Role of Epigenetic Regulation and HDAC Inhibition. Antioxid Redox Signal.. 2015. 22(16). 1382-1424.
Palliyaguru DL, Yang L, Chartoumpekis DV, et al. Sulforaphane Diminishes the Formation of Mammary Tumors in Rats Exposed to 17β-Estradiol. Nutrients. 2020. 12(8). 2282.
Mayra ST, Johnston CS, Sweazea KL. High-nitrate salad increased plasma nitrates/nitrites and brachial artery flow-mediated dilation in postmenopausal women: A pilot study. Nutr Res. 2019 May;65:99-104. doi: 10.1016/j.nutres.2019.02.001. Epub 2019 Feb 22. PMID: 30954341.
https://aacrjournals.org/cebp/article/9/8/773/179852/Brassica-Vegetable-Consumption-Shifts-Estrogen
Liu ZM, Ho SC, Xie YJ, et al. Whole plant foods intake is associated with fewer menopausal symptoms in Chinese postmenopausal women with prehypertension or untreated hypertension. Menopause. 2015;22(5):496-504. [PMID:25387345]
Beezhold B, Radnitz C, McGrath RE, et al. Vegans report less bothersome vasomotor and physical menopausal symptoms than omnivores. Maturitas. 2018;112:12-17. [PMID:29704911]
Kroenke CH, Caan BJ, Stefanick ML, et al. Effects of a dietary intervention and weight change on vasomotor symptoms in the Women’s Health Initiative. Menopause. 2012;19(9):980-8. [PMID:22781782]
Yim G, Ahn Y, Chang Y, et al. Prevalence and severity of menopause symptoms and associated factors across menopause status in Korean women. Menopause. 2015;22(10):1108-16. [PMID:25783469]
Murkies AL, Lombard C, Strauss BJ, et al. Dietary flour supplementation decreases post-menopausal hot flushes: effect of soy and wheat. Maturitas. 2008;61(1-2):27-33. [PMID:19434877]
Lewis JE, Nickell LA, Thompson LU, et al. A randomized controlled trial of the effect of dietary soy and flaxseed muffins on quality of life and hot flashes during menopause. Menopause. 2006;13(4):631-42. [PMID:16837885]
Lethaby A, Marjoribanks J, Kronenberg F, et al. Phytoestrogens for menopausal vasomotor symptoms. Cochrane Database Syst Rev. 2013. [PMID:24323914]
Franco OH, Chowdhury R, Troup J, et al. Use of Plant-Based Therapies and Menopausal Symptoms: A Systematic Review and Meta-analysis. JAMA. 2016;315(23):2554-63. [PMID:27327802]
Chen MN, Lin CC, Liu CF. Efficacy of phytoestrogens for menopausal symptoms: a meta-analysis and systematic review. Climacteric. 2015;18(2):260-9. [PMID:25263312]
Barnard ND, Kahleova H, Holtz DN, Del Aguila F, Neola M, Crosby LM, Holubkov R. The Women’s Study for the Alleviation of Vasomotor Symptoms (WAVS): a randomized, controlled trial of a plant-based diet and whole soybeans for postmenopausal women. Menopause. 2021 Jul 12. doi: 10.1097/GME.0000000000001812. Epub ahead of print. PMID: 34260478.
Messina M. Soy foods, isoflavones, and the health of postmenopausal women. Am J Clin Nutr. 2014 Jul;100 Suppl 1:423S-30S. doi: 10.3945/ajcn.113.071464. Epub 2014 Jun 4. PMID: 24898224.
Jull J, Stacey D, Beach S, Dumas A, Strychar I, Ufholz LA, Prince S, Abdulnour J, Prud’homme D. Lifestyle interventions targeting body weight changes during the menopause transition: a systematic review. J Obes. 2014; 824310.
Kapoor E, Collazo-Clavell ML, Faubion SS. Weight Gain in Women at Midlife: A Concise Review of the Pathophysiology and Strategies for Management. Mayo Clin Proc. 2017 Oct;92(10):1552-1558.
Lonnie M, Hooker E, Brunstrom JM, Corfe BM, Green MA, Watson AW, Williams EA, Stevenson EJ, Penson S, Johnstone AM. Protein for Life: Review of Optimal Protein Intake, Sustainable Dietary Sources and the Effect on Appetite in Ageing Adults. Nutrients. 2018 Mar 16;10(3):360. doi: 10.3390/nu10030360..
Simpson SJ, Raubenheimer D, Black KI, Conigrave AD. Weight gain during the menopause transition: Evidence for a mechanism dependent on protein leverage. BJOG. 2023 Jan;130(1):4-10.
Nie, X., Xie, R. & Tuo, B. (2018). Effects of Estrogen on the Gastrointestinal Tract. Dig Dis Sci 63, 583–596.
Siddiqui, R.; Makhlouf, Z.; Alharbi, A.M.; Alfahemi, H.; Khan, N.A. The Gut Microbiome and Female Health. Biology 2022, 11, 1683. https://doi.org/10.3390/biology11111683
Veira, A.,
Castelo, P. et al, (2017). Influence of oral and gut microbiota in the health of menopausal women. Front. Microbiol. 8: 1884
Baylis, D., Bartlett, D.B., Patel, H.P. et al. (2013). Understanding how we age: insights into inflammaging. Longev Healthspan 2, 8. https://doi.org/10.1186/2046-2395-2-8
Ferrucci L. & Fabbri, E. (2018). Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nat Rev Cardiol. 15(9):505-522. doi: 10.1038/s41569-018-0064-2. PMID: 30065258; PMCID: PMC6146930.
Franceschi, C. et al. (2018) Inflammaging: a new immune-metabolic viewpoint for age-related diseases. Nat. Rev Endocrinology, 14(10):576-590.
McCarthy M, Raval AP. The peri-menopause in a woman’s life: a systemic inflammatory phase that enables later neurodegenerative disease. J Neuroinflammation. 2020 Oct 23;17(1):317.
Neves J., & Sousa-Victor, P. (2020). Regulation of inflammation as an anti-aging intervention. FEBS J. 287(1):43-52. doi: 10.1111/febs.15061 31529582.
McCarthy, M., Raval, A.P. The peri-menopause in a woman’s life: a systemic inflammatory phase that enables later neurodegenerative disease. J Neuroinflammation 17, 317 (2020). https://doi.org/10.1186/s12974-020-01998-9
Aslani Z, Abshirini M, Heidari-Beni M, Siassi F, Qorbani M, Shivappa N, Hébert JR, Soleymani M, Sotoudeh G. Dietary inflammatory index and dietary energy density are associated with menopausal symptoms in postmenopausal women: a cross-sectional study. Menopause. 2020 May;27(5):568-578. doi: 10.1097/GME.0000000000001502. PMID: 32068687.
Davis, S., Castelo-Branco, C. et.al. (2012). Understanding weight gain at menopause. Climacteric, 15: 419–429.
Reinke H. & Asher G. (2017). Circadian clock control of liver metabolic functions. Gastroenterology, 150: 574–580.
North American Menopause Society (12th Oct. 2022). Hot flashes are not just uncomfortable but also could be hard on the heart
Kodoth V, Scaccia S, Aggarwal B. Adverse Changes in Body Composition During the Menopausal Transition and Relation to Cardiovascular Risk: A Contemporary Review. Womens Health Rep (New Rochelle). 2022 Jun 13;3(1):573-581.
Biglia N, Cagnacci A, Gambacciani M, et al. Vasomotor symptoms in menopause: a biomarker of cardiovascular disease risk and other chronic diseases? Climacteric. 2017;20(4):306-312. [PMID:28453310]
Franco OH, Muka T, Colpani V, et al. Vasomotor symptoms in women and cardiovascular risk markers: Systematic review and meta-analysis. Maturitas. 2015;81(3):353-61. [PMID:26022385]
Lee, E., Anselmo, M, Tahsin, T. et al. Vasomotor symptoms of menopause, autonomic dysfunction, and cardiovascular disease. 2022, Am. J. of Physiology
Stachowiak G, Pertyński T, Pertyńska-Marczewska M. Metabolic disorders in menopause. Prz Menopauzalny. 2015 Mar;14(1):59-64. doi: 10.5114/pm.2015.50000. Epub 2015 Mar 25.
Daley A, Stokes-Lampard H, Thomas A, et al. Exercise for vasomotor menopausal symptoms. Cochrane Database Syst Rev. 2014. [PMID:25431132]
Daley A, Macarthur C, Stokes-Lampard H, et al. Exercise participation, body mass index, and health-related quality of life in women of menopausal age. Br J Gen Pract. 2007;57(535):130-5. [PMID:17266830]
Ayers B, Smith M, Hellier J, et al. Effectiveness of group and self-help cognitive behavior therapy in reducing problematic menopausal hot flushes and night sweats (MENOS 2): a randomized controlled trial. Menopause. 2012;19(7):749-59. [PMID:22336748]
Daley A, Stokes-Lampard H, Macarthur C. Exercise for vasomotor menopausal symptoms. Cochrane Database Syst Rev 2011 5:CD006108.
Carpenter JS, Burns DS, Wu J, Otte JL, Schneider B, Ryker K, Tallman E, Yu M. Paced respiration for vasomotor and other menopausal symptoms: a randomised controlled trial. J Gen Intern Med 2013 28:193–200.
Woods, N. et al. (2009). Cortisol Levels during the Menopausal Transition and Early Postmenopause: Observations from the Seattle Midlife Women’s Health Study. Menopause, 16(4): 708–718
Saensak S, Vutyavanich T, Somboonporn W, et al. Relaxation for perimenopausal and postmenopausal symptoms. Cochrane Database Syst Rev. 2014. [PMID:25039019]



