What you can do for long COVID recovery part 1: nutrition, gut health and stress
By Dr Marissa Kelaher, graphics by Dr Taisia Cech
Do you, or someone you know, have long COVID or post COVID-19 symptoms?
If so this post is for you!
With COVID-19 becoming endemic in New Zealand, long COVID and post COVID symptoms are a growing issue. Estimated to affect between 30 to 50% of people who have COVID-19, it's an area of research that's developing constantly - as we discover more about what causes it, and what might help.
As its a huge topic, we've divided it into two blog posts - this one covers nutrition, stress, dizziness, palpitations, and cognitive symptoms (brain fog) - part 2 covers exercise and fatigue.
WHAT IS LONG COVID?
While long COVID is often used to describe any persistent symptoms 4 weeks after acute COVID-19 infection, in reality there are actually three different types :
ongoing symptomatic COVID-19 infection (which lasts from 4 weeks post COVID-19 infection to 12 weeks)
post COVID syndrome, where symptoms last more than 12 weeks, can fluctuate, and are NOT due to ongoing infection (but rather cluster of symptoms after the initial infection has resolved)
long COVID, which actually includes both of the above
Symptoms are hugely variable, reflecting how widely the COVID-19 virus affects our body.
The most common ones are fatigue, shortness of breath and cough, heart palpitations and chest tightness /pain, headache, and brain fog. Other symptoms can include sleep disturbances, dizziness, joint and muscle pain, loss of taste/smell, pins and needles, earache or sore throat, tummy upset, or even persistent fever
WHAT CAUSES LONG COVID?
We are still finding out exactly what causes long COVID, but current theories are :
the direct effect of the virus on our cells
the persistence of viral fragments in our body that continue to trigger symptoms
an abnormal (overactive) immune response, causing chronic inflammation
Of these three, chronic inflammation is a theory that's currently gaining the most traction, as it helps to explain the huge range of body systems affected.
Long COVID can occur in anyone infected with COVID-19, and isn't particularly linked with how severe the initial infection is.
Risk factors include:
older age
having more than one underlying chronic medical condition
a higher body mass index (obesity)
being female
being admitted to hospital during acute phase of having COVID 19
Vaccination significantly reduces the risk of developing long COVID and is the most important way to prevent it - but gut health, diet, and lifestyle factors also play a role.
Once you develop long COVID symptoms, the focus becomes very much on lifestyle interventions to manage symptoms and allow your body to gradually recover - so lifestyle medicine is a perfect fit!!!
Note : this advice is designed to be used in conjunction with medical care, and AFTER being medically cleared by your doctor. If you have severe symptoms (fatigue, headache, breathlessness, racing heart, dizziness, or confusion) then PLEASE see your doctor first to rule out other potential causes, and do not start exercise until medically cleared to do so. A physical exam, as well as potentially blood tests, an ECG, or a chest x-ray, or other testing may be needed depending on your symptoms
A LIFESTYLE MEDICINE APPROACH TO LONG COVID
Since chronic inflammatory processes are thought to be one of the main potential mechanisms behind long COVID, treatments and rehabilitation strategies aim to reduce this chronic inflammation, as well as rebuilding strength and energy levels.
These are divided into :
anti-inflammatory nutrition
restorative sleep
stress management, and tools to modify the stress and nervous system response, such as yoga and breathing
structured gentle paced exercise
energy management
Let's look at each of these in more detail now
NUTRITION
Research into COVID-19 consistently shows that diets that are high in whole plant foods, fibre, and antioxidant foods, and low in 'inflammatory' foods appear to protect against severe COVID-19 infection,and may also help in long COVID recovery.
These are often also called blue zones or Mediterranean diets, which are in reality very similar, as they all focus on whole foods, and are mostly plant based.
Their effect on COVID-19 is thought to be due to several main factors - the direct role of food in regulating inflammation, the presence of adequate micronutrients that are needed for effective immune function, and the effect of food on the gut microbiome. These are actually all interconnected - with food, inflammation and our gut microbiome affecting one other.
anti-inflammatory diet
As mentioned previously, chronic inflammation is thought to play a significant role in COVID-19 infection. As a result, nutrition treatment aims to reduce this inflammation, via following specific dietary patterns.
The dietary inflammatory index is a well validated tool that's been used to look at diet in various diseases, as it measures how different foods can cause inflammation in the body. There are over 6000 published studies on the DII!!
The following graphic shows the DII in relation to common foods, and how ‘inflammatory’ they are, it is an excerpt from the diet and inflammation section of our Nutrition and Reboot courses. .
The more negative a score, the more anti-inflammatory a food is, while more positive scores are more inflammatory.
Research looking at diet and COVID-19 have shown that both plant based diets and 'anti inflammatory' diets as per the DII, can significantly reduce the risk of severe COVID-19. They are also thought to improve long COVID recovery, and although the research on this is still limited, it makes biological sense for the reasons mentioned.
Plant based diets and anti-inflammatory diets help improve other inflammatory conditions, and are proven to be beneficial for overall health, heart health, brain health, mental health, metabolic health, longevity and more. Plant based diets and anti-inflammatory diets have also been shown to help conditions associated with long COVID, such as fatigue, sleep disturbance, mood disturbance, pain and chronic inflammation.
Population studies of plant based diets for example, found a whopping 67% reduced risk of severe COVID-19 in people who ate plant based (vegan or vegetarian) diets!
This is thought to be related to the high levels of anti-inflammatory compounds (antioxidants and polyphenols) in plant based diets, the effect of high fibre levels on improving the gut microbiome, the lack of inflammatory foods, and their effect on reducing rates of other health issues associated with a higher risk of severe COVID-19.
In reality anti - inflammatory diets and whole food plant based diets also are very similar - as whole plant foods (in particular brightly colored fruit and veges) are highly anti-inflammatory. Foods rich in omega 3 (nuts, seeds, and oily fish) are also anti - inflammatory, while animal based foods (in particular red meat), refined grains, added sugars, and processed foods are considered inflammatory.
They are often also called Mediterranean diets, and although there are slight variations between the three diets, they are similar enough to use this as an overall guide. The pictures below are from our Nutrition module and Reboot course, and give a guide on both what foods to include, as well as how to balance your plate.
Plant based diets, anti-inflammatory diets, and Mediterranean diets all emphasize vegetables, legumes, fruits, whole grains, nuts, herbs, and seeds as the main food sources.
These are:
high in fiber, antioxidants, and phytochemicals (‘anti-inflammatory’ nutrients)
low in cholesterol, haem iron, saturated fat, and animal proteins ( ‘pro-inflammatory’ nutrients)
low in refined carbs, alcohol, added sugar, trans fat, and ultra-processed foods ( ‘pro-inflammatory’ nutrients)
contain adequate micronutrients needed for healthy immune function, in particular vitamin C, vitamin A, zinc, and omega 3.
To eat an anti-inflammatory diet, try to eat mostly whole unprocessed foods, and remember the phrase 'eat a rainbow' - aiming for a big diversity of different coloured plant foods, and with very little red meat, saturated fat, added sugar, alcohol, refined carbs and processed foods.
Or in Michael Pollans famous words ‘Eat whole foods, mostly plants, not too much!!
OTHER TIPS:
Make sure you stay well hydrated, choosing unsweetened drinks such as water, herbal tea, or green tea.
Eat foods with a lower glycemic index (ie less effect on blood sugar) to help reduce fatigue, POTS (postural orthostatic tachycardia syndrome - see below) and brain fog, and to reduce inflammation - again these are whole plant foods, unsaturated fats, and high quality protein such as legumes, fish, and eggs /chicken /some dairy if desired.
If you'd like to know more about this diet in detail, check out our longevity blog post here, or our Transform your Nutrition and Reboot your Health courses .
This dietary pattern is also shown to help with depression and anxiety, as well as cognitive issues ('brain fog') which are common symptoms of long COVID.
Please see our blog post on eating for mental health for more details.
We cover all of these areas in detail in our Transform your Nutrition and Reboot your Health courses .
gut health
Gut health also appears to play a potential role in both long COVID and severe COVID-19, with risks of both inked to reduced gut microbiome diversity. Again the research on this is limited, but given what we know about the importance of gut health in a healthy immune system, and in regulating inflammation, it makes total sense.
Eating a diet based around whole plant foods, rich in fibre, with a big diversity of different plants (ie 30 different plant foods each week), and including fermented foods, helps to optimise our gut microbiome, and is the only ‘gut health diet’ actually backed by scientific research.
We love the 30+ a week concept - aiming to include 30 different whole plant foods in your diet each week - proven to create the greatest gut microbiome diversity!
In contrast, ultra-processed foods, refined carbs, red meat, and saturated fat can all potentially reduce gut microbiome health, so its best to avoid or limit these if possible.
Avoiding unnecessary antibiotics or medications, and disinfectants, and practicing healthy lifestyle habits also help our gut health and gut microbiome - see our gut blog post or our Nutrition or Reboot courses for more details. The graphic below is from these, showing how to balance your diet for optimal nutrition.
STRESS REDUCTION
Long COVID can affect both mood and our autonomic nervous system (due to stress around being unwell, the effect of inflammation on our mood, and the direct effects of covid on our nervous system).
Dysautonomia (a dysregulation of the autonomic nervous system) is extremely common in long COVID, and can result in a range of symptoms . Tachycardia, orthostatic hypotension, and POTS are all thought to be due to dysautonomia ie our nerves not responding to physical and emotional challenges the way the way they should (even a change in position from sitting to standing, or a poor night's sleep can trigger symptoms).
Stress reduction and strategies to 'calm our stress response' and activate our ‘rest and digest’ (vagus nerve and parasympathetic nervous system) are therefore a crucial part of recovery from long COVID.
In addition, dysfunctional breathing (shallow or fast breathing) is also very common in long COVID, and can worsen symptoms - so many long COVID recovery programs focus on improving breathing techniques as well as physical exercises - in particular emphasising the importance of slow controlled diaphragmatic breathing (see below). These have the added benefit of activating our vagus nerve and improving our autonomic nervous system function.
Strategies to help reduce stress include:
altering our stress response and perception (ie how we react to stresses)
building stress resilience (how our body and mind cope with physical and mental stress)
using breathing techniques to help retrain our nervous system and lungs.
practical tips to reduce stress
limit what you are exposed to - avoid watching too much news or social media if its making you feel anxious.
stay in touch with family and friends, and surround yourself with people you can confide in, trust, and who help you feel more positive
try to do activities that you find enjoyable and relaxing.
don’t be too hard on yourself if there are things that you are finding harder to do, and remind yourself that recovery takes timer
practice self compassion
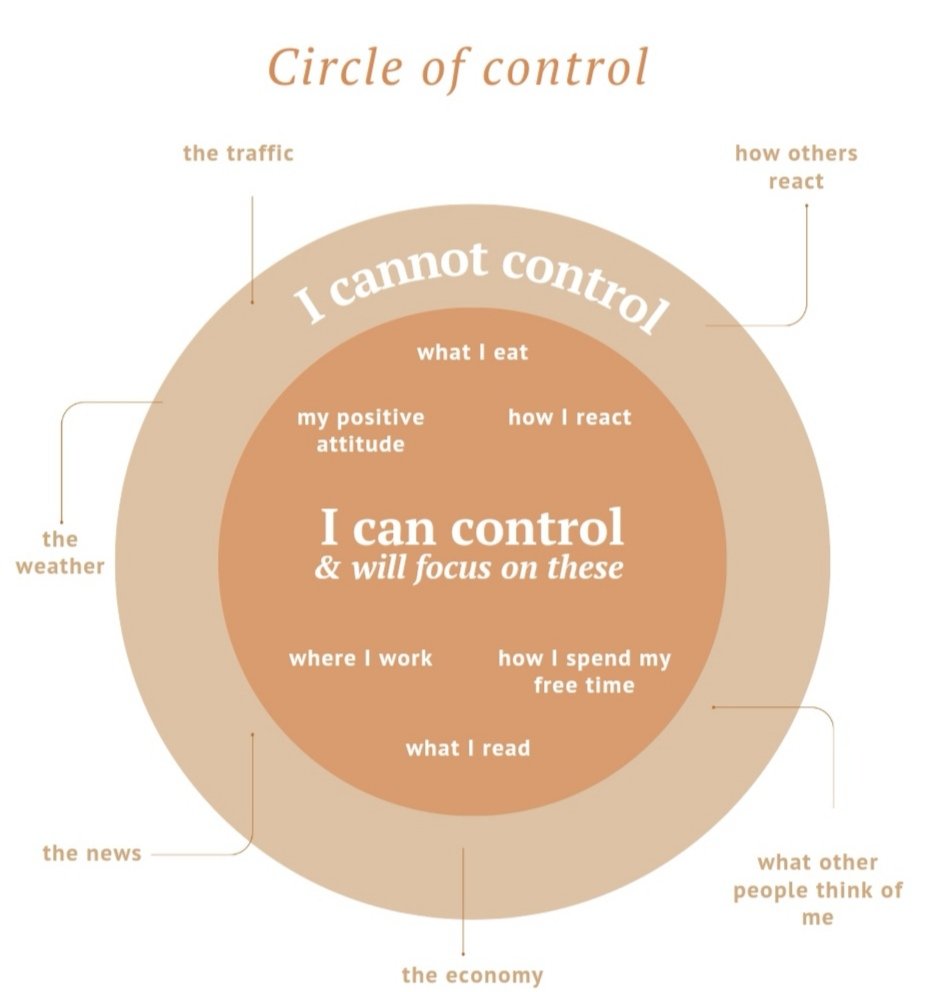
focus on what is in your control, rather than what is not. This graphic is from our Take control of your stress and Reboot courses, it's also included in our free mini stress booklet in the “free stuff’ page of our website
Another tip is to use gratitude practicing to change your focus, this can interrupt cycles of negative thoughts.
To do this, try to deliberately think of 3 things you are grateful for each time your thoughts start to spiral out of control or get into a negative pattern. Over time this can actually re-wire your brain!
relaxation and grounding techniques
These are also great ways to reduce stress and calm your nervous system. They can help control anxiety, improve quality of life and sleep, and reduce pain. Gentle yoga, progressive muscle relaxation, guided meditation, time in nature, and mindfulness are all good techniques to use.
We have a free Stress reduction mini e-book here for download that covers the basics, or you can check out our Take control of your stress module or Reboot course where we explore these in detail.
You can also try the following techniques when your heart or breathing speeds up or you feel stressed:
GROUNDING:
Take 3 slow deep breaths and ask yourself:
1. What are five things I can see?
2. What are four things I can feel?
3. What are three things I can hear?
4. What are two things I can smell?
5. What is one thing I can taste?
Think of the answers slowly to yourself, one sense at a time and spend at least ten seconds focusing on each one, while continuing to take slow deep breaths. Then notice how your body and mind feel. Repeat as often as needed, over time this will help to reduce overwhelm, stress, and clear your mind.
BREATHING:
1. Get in a comfortable position, either seated or on your back.
2. Close your eyes and bring your attention to your breathing.
3. Breathe in and out through your nose (or mouth if you are unable to do this - but work towards trying to breathe through your nose eventually).
4. Put a hand on your stomach and recognise how it rises and falls when you breathe in and out.
5. Try to breathe in for the count of one, PAUSE and then out for count of two, working towards a longer breath out than in. This will slow your breathing rate down and activate your vagus nerve, the ‘rest and digest ‘part of your nervous system.
6. Notice areas of tension in your body and try to release this with each breath out. You can start at your feet and slowly bring attention up your body, consciously relaxing each area in turn.
7. Gradually try to make your breaths slower and deeper, keeping the exhale longer than the inhale.
Try our 5 minute breathing video here for more guidance (if you find the breath hold and exhale too long at first, start with 3 or 4 seconds).
We also teach breathing techniques and guided relaxation meditations in our Stress Module and Reboot course. The graphic below is from these courses.
Pursed lip breathing (taking long slow breaths out against pursed lips) can also help improve your lung function and nervous system, as it exercises your diaphragm (main breathing muscle).
More exercises and details here
other strategies for postural dizziness and POTS
There are also additional practical strategies that can help with postural dizziness/orthostatic hypotension or POTS such as:
avoiding rapid changes in position or activity
staying well hydrated and adding extra electrolytes to fluids to help blood volume (ie rehydration sachets)
wearing lower limb compression stockings
eating small regular low GI meals more often (to avoid blood sugar crashes)
including complex carbs and fibre in each meal
limiting added sugar, refined carbs and alcohol
exercising while lying flat, sitting, or reclining initially if standing worsens symptoms.
Sleep is also extremely important, please see our sleep blog for tips on improving sleep, or checkout our Restorative Sleep module or full Reboot course where we cover sleep in depth.
BRAIN FOG AND MENTAL FATIGUE:
Brain fog and mental fatigue can be some of the most disabling symptoms of long COVID, and are often what affect peoples ability to work and function. A feeling of overwhelming mental fatigue, as well as trouble concentrating, making decisions, planning, and multitasking are all typical symptoms, and can have a massive impact on quality of life.
Physical fatigue is also a huge issue in long COVID, we cover this in our second blog post. We aren't fully sure why this occurs so much in long COVID- the theories mentioned at the start of this post are thought to play a role, as well as potentially mitochondrial dysfunction (mitochondria are the energy production part of our cells).
Strategies to help with brain fog and mental fatigue include anti-inflammatory nutrition, stress reduction, and prioritising sleep as discussed, as well as specific tips to reduce the energy needs of our body and mind. We cover all of these in our Focus Modules and Reboot course
The area of our brain that we need for planning, decision making and concentration (the prefrontal cortex) , is also the most energy intensive part- so it tires fastest, and is therefore affected the most by long COVID, lack of sleep, imbalanced nutrition, and stress.
Using strategies to reduce the 'load' can help your brain and body recover faster, and help you feel better
SOME PRACTICAL TIPS INCLUDE:
Minimise distractions: Try to work in a quiet environment with no distractions. This reduces the need to multitask and switch attention, which uses extra energy
Regularly switch off technology and limit screen time, this is energy draining due to the level of mental stimulation it creates. Turn off notifications on apps, as these create distractions and force us to switch our attention back and forth
If you are distracted when reading, block off parts of the text using paper, or use your finger as a marker, so you can focus on a bit at a time.
Be conscious of your brain needing rest, and try plan things that require concentration for times when you are less tired. For example if you tire as the day goes on - then do this task in the morning. Think of your brain as a muscle that needs breaks as well, and build in rest periods, especially when doing more intensive tasks
Say things out loud or write them down to help you remember them: Saying things out loud like ‘what should I be doing now?’ or ‘Stay focused’ can help you stay on track when you are struggling to concentrate
Take frequent breaks: try work for shorter periods of time and take breaks, be kind to yourself. Use “little and often” as a guide and pace yourself.
Set yourself targets or goals: Having something definite to work towards will help you stay motivated. Set clear specific deadlines like “I’ll do that task at 10 o’clock”, instead of “I’ll do my work later on”. We teach goal setting, practical ways to create healthy habits, and how to break activities into small steps in detail in our behaviour change module and Reboot course.
Try creating a regular daily/weekly schedule to reduce the need for planning and decision making. Keep a record, or break things down into small sections, so if you get distracted you can pick up where you left off.
Use lists, diary's, alarms, or apps to help reduce the amount you need to remember, this can also reduce the stress of worrying you'll forget things. Lists are your friend!
Use incentives: When you achieve a target or goal reward yourself, reward yourself with something healthy you enjoy, such as a rest, a gentle walk, listening to music, or a herbal tea. Practice self compassion
Avoid multitasking. Concentrate on one thing at a time, do not try to take in too much information at once, as this can lead to mistakes. Do one task then move on to the next.
Don’t rush things: You may find that you have a tendency to rush everyday tasks and end up making mistakes. Take your time and pace yourself.
Gain control: If in conversations you feel you are being ‘overloaded’, ask the person who is talking to you to slow down and/or repeat themself. It's OK to be assertive and say ‘Excuse me, I think you have lost me, could you repeat that please?’
Repeating things: Immediately repeating something or writing it down after hearing it can help imprint it in your memory
Find ways to learn that are easier on your brain - for many people listening to books or podcasts can be easier than reading text. Take advantage of the options out there.
And remember - success is gained in small gradual steps, rather than large leaps!
If you are feeling overwhelmed, just start with one or two small habits you can do on a daily basis, and do these consistently for a week or two before adding a couple more healthy habits.
It’s what you do on a daily basis that has the most impact over the long term - every little step counts, and even though it may not feel like it, over time these are what lead to healing, recovery, and true change ❤️
We teach this in detail, as well as how our brains work, and how to use this knowledge to make change easy in our behaviour change module and Reboot course
To learn how to manage exercise and physical fatigue in long COVID, please check out part two of our blog here.
REFERENCES AND FURTHER READING:
https://gh.bmj.com/content/6/9/e005427.long
https://www.nice.org.uk/guidance/ng188/resources/covid19-rapid-guideline-managing-the-longterm-effects-of-covid19-pdf-51035515742
Gut microbiome and long COVID: https://gut.bmj.com/content/71/3/544; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8478109/
Gut microbiome and severe COVID-19:
https://gut.bmj.com/content/70/4/698
https://www.sciencedirect.com/science/article/pii/S2590097820300203?via%3Dihub
Plant based diets and risk of COVID-19 and long COVID:
https://gut.bmj.com/content/70/11/2096
https://pubmed.ncbi.nlm.nih.gov/34308134
Plant based diets as treatment for long COVID: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8429479/
COVID-19 and DII: https://pubmed.ncbi.nlm.nih.gov/34420546/
https://www.mdpi.com/2079-9721/9/4/76/htm
NHS Your COVID recovery: https://www.yourcovidrecovery.nhs.uk/
• Older people: https://library.nhs.uk/coronavirus-resources/older-people/
• Children and young people: https://library.nhs.uk/coronavirus-resources/children-and- young-people/
• How to manage post-viral fatigue after COVID-19: https://www.rcot.co.uk/how-manage-post-viral-fatigue-after-
covid-19
• Long COVID-19 Foundation: www.longcovidfdn.com
Long covid symposium recording NZ: https://events.otago.ac.nz/longcovid2022/
Breathing guidelines: https://onlinelibrary.wiley.com/doi/10.1002/pmrj.12744
Cognitive symptoms guidelines: https://onlinelibrary.wiley.com/doi/10.1002/pmrj.12745